This is the second in a series of blogs on governance and the benefits of mechanised assurance. The content is taken from a Good Governance Institute whitepaper, developed with Allocate with contributions from NHS colleagues.
“Boards need to be confident that the systems, policies and people they have put in place are operating in a way that is effective, is focused on key risks and is driving the delivery of objectives.”
To ensure that a board is confident that its organisation is delivering its strategic objectives as well as high-quality care for patients on a day to day basis, NHS organisations need to have in place an assurance system that the board can be confident in. Without some kind of robust assurance system, the board will not be able to understand the myriad elements of what is going on in the organisation at any one time. The assurance system should continually inform the board of performance data, principal risks facing the organisation and significant aspects of regulatory compliance. However, the term ‘assurance’ can often be misunderstood, and the concept difficult to define. This confusion may well be augmented by the fact that, at present, there are no national guidelines for assurance in the NHS.
What is assurance and why is it so important?
Assurance could be described as ‘a positive declaration that a thing is true’. Assurance is therefore the information and evidence provided or presented to a board, which is intended to stimulate confidence that everything in the organisation is as it should be, even though they may not have witnessed this for themselves.13 For example, the Airedale Inquiry into nursing failures at Airedale NHS Trust, found:
‘The most striking failure was in the disconnection between what was happening on the wards at night, and what the Board knew. The Board had no idea.’
The deaths of the patients at the heart of this scandal occurred on the wards during the night: the Board never would have seen what was going on. However, it should have had assurance that someone knew what was going on and acted on this.15 This represents a striking failure in the assurance processes in this hospital.
Therefore, assurance is the process by which organisations demonstrate that they are operating effectively and achieving performance. This includes:
- Delivering targets and objectives
- Preventing and managing risk
- Following best practice
- Meeting needs of patients
- Complying with statutory, regulatory and other requirements
Essentially, assurance is the generation and delivery of accurate and up to date information about the ‘efficiency and effectiveness of an organisation’s policies and operations, and the status of its compliance with statutory obligations. Assurance is the process of establishing the integrity and validity of disclosures, including statements and reports.’ Effective assurance relies upon the quality of evidence, which should assure the board that performance and the quality of care are consistent with national and organisational standards, that risks are properly controlled and that the strategic objectives are being achieved. In order to validate this evidence, assurance should come from more than one source.
Sources of assurance include:
Data and information
- Reports and briefings
- Comparative data and statistics
- Comparison and benchmarking over time, both internally and externally
- Provision of evidence that data is reliable and accurate
People
- Talking to staff and patients
- Asking questions in order to validate the data and information provided in reports and briefings
Observation
- Taking a staff member’s and/or patient’s eye-view
- Structured visits, walkabouts, case studies, in order to learn what is actually happening throughout the organisation
- Comparison of the data and the outcomes of observations – do they correlate?
- Deep dives
With the wide range of data that is now required to be collected by NHS trusts, there is a benefit in triangulating this information and evidence to ensure that a single, consistent version of the truth is presented both internally and externally.
The value of assurance
Although assurance has long been considered an integral aspect of governance, in recent years boards have had more of an onus placed upon them to ensure that they are confident of the performance, both in terms of financial sustainability and clinical quality, of the organisations which they lead. Chief executives in NHS trusts are required to sign, on behalf of their boards, an annual governance statement. This covers, for example, the governance framework of the organisation, risk assessment, the risk and control framework, and the review of the effectiveness of risk management and internal control.17 To provide this, boards therefore need to be able to demonstrate that they have been properly informed through assurances about the true picture of their risks, and, based on the evidence presented to them, have made appropriate conclusions.
When effective assurance systems are not in place, the board may not be able to fulfil its internal scrutiny, with what the board believes is happening being very different to what is actually happening in the wards. Various studies, for example on hospital acquired infections and compliance with employment checks, have demonstrated that boards may report compliance with standards, when in fact they are not being delivered in practice,suggesting that the systems in place are not providing adequate assurance.
“This is not just a case of mendacity of boards, but almost a worst state of affairs – boards are genuinely unaware that standards they claim are being met are not being delivered in practice universally consistently.”
An example might be the regulatory requirement to ensure that all employed staff meet training and review requirements whereas the board might reasonably want assurance that these requirements are also met by agency and visiting staff who are not employed by the trust.
High profile failings of care have demonstrated this disconnect, as for example in the events at Mid Staffordshire NHS Foundation Trust. The Francis Report into the failings concluded that the board had had a ‘vestigial’ clinical governance system, and therefore were ‘blind’ to the concerns that were then raised by the Healthcare Commission’s investigation in 2009.21 Assurance needs to provide a clear line of communication between the ward and the board. While the concept of assurance being ward to board being well known in the NHS, it has been suggested to us that in fact assurance should be ward to board and beyond. NHS board members have an ethical and moral duty in their role, to look after something that is not theirs, and aim to leave it in a better place than they found it. With this in mind, the public are looking to the board of NHS organisations to assure them about the condition and performance of local NHS services. Assurance systems should be able to facilitate this link.
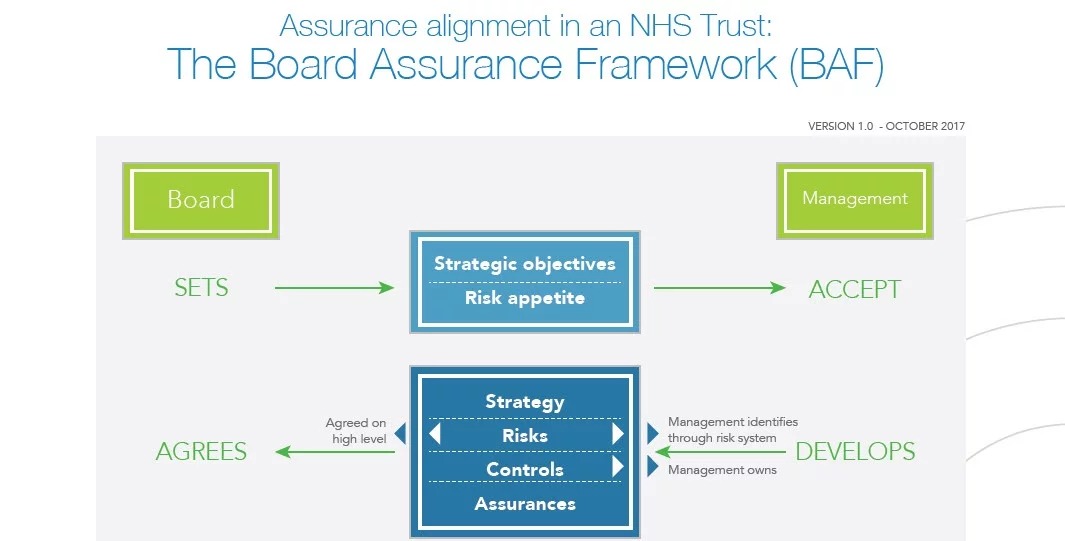
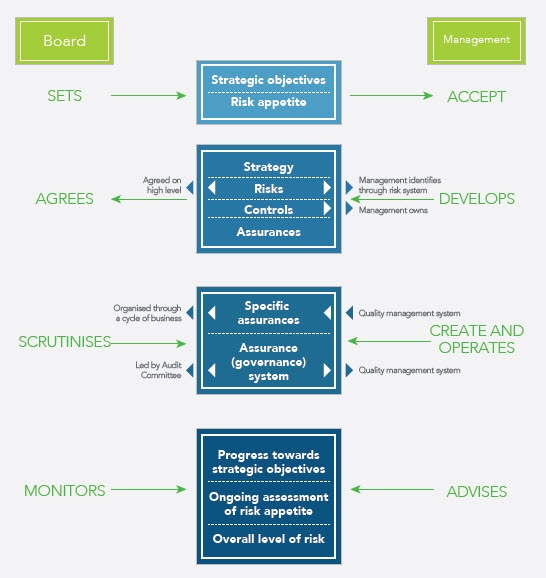
The ‘Board Assurance Framework’ (BAF) is a principle mechanism by which a board tracks focus on the progress of the organisation’s strategic objectives and keeps an eye on and mitigates against any risks that may hinder the achievement of these objectives. In addition to the BAF, boards of healthcare organisations also need to be confident that there are effective systems in the place for the following, which are collectively known as assurance systems:
- To endorse, monitor and develop appropriate policies and guidance for the management of the organisation and the minimisation of risk
- To report and monitor progress against both the strategy and the business plan
- To identify and assess risks and hazards, and act accordingly
- To ensure that the required compliances are maintained
Assurance should not offer just a retrospective view of what is going on in the organisation, but a progressive and forward looking view of performance, able to support with both the analysis of trends and the projecting of trajectories. It makes sense that an organisation that is better able to identify where a deterioration in performance or quality and safety of care may occur will then be better positioned to deploy the resource and extra support necessary to mitigate any negative impact upon patients, compliance, and the delivery or consequent modification of strategic objectives. Many board papers in the NHS currently do not project forward trend lines, perhaps due to the difficulty felt by many in the NHS in converting data into useful information. Meanwhile, an effective assurance system should weave together evidence around, for example, quality, finance, workforce and partnerships, rather than dealing with them in siloes.
In the NHS of the 21st century what is the most effective and efficient way for organisations and their boards to ensure this model of assurance is being delivered? However assurance evolves, the process should be simple and able to facilitate a genuine culture of quality improvement. In the words of one NHS Chief Operating Officer:
“It would be helpful ‘for everything to be a little bit more simple… we just keep feeding the beast and I don’t see it stopping, I just see it getting worse”
Assurance alignment in an NHS Trust: The Board Assurance Framework (BAF)
Request the full whitepaper or subscribe to the blog to receive an email notification when the next excerpt is published.

Andrew Corbett-Nolan is the Chief Executive of GGI, and has worked in healthcare since joining the NHS in 1987. He specialises in board development work, and some of the more complex governance reviews that GGI undertakes. Visit http://www.good-governance.org.uk/ to find out more about the GGI